Caring for someone with a dual diagnosis of paranoid schizophrenia and dementia
- 25 September 2023
- 9 min read
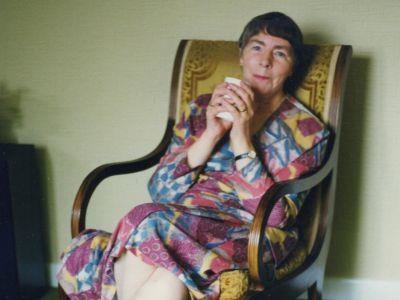
This blog tracks living with and then caring for a mother with paranoid schizophrenia who later was also diagnosed with mixed dementia and latterly Alzheimer’s disease. It is a personal story, but also includes a list of relevant studies and papers. Each person’s account of caring for someone with dementia is unique. I hope this blog will be familiar to other carers and for researchers to confirm your thoughts, spark debate or inspire ideas for future and current research. The references are a snapshot of research to help me and others understand what my family experienced. All comments and questions welcome.
Part 1 The dual diagnosis of paranoid schizophrenia and dementia
As a young child, I could not understand why my mother’s outlook on life caused issues in our household as other adults challenged my mother’s narratives. As I grew older, I realised my mother’s perceptions would cause problems for me outside the home.
After forty-five years of marriage, my father left the family home for a new life elsewhere. He had a long struggle trying to support my mother who was not receptive to his attempts to help, as well as being exhausted by being at the centre of her delusions. Mum had no insight into her paranoid schizophrenia maintaining that she had no illness and a narrative that was to haunt her all her life. As a result, she was in a revolving door process of taking medication (which changed due to current trends and developments over the years), deciding she did not need drug therapy, and then ending up in hospital again, always on a section and always against her will.
Mum was fiercely protective of her children, but I chose to break free, while she and my brother (also later diagnosed with autism and paranoid schizophrenia) maintained a close relationship until mum began to lose her memory and mobility as a result of dementia. My brother could not cope with mum’s dementia while, oddly, it brought mum and I closer together.
I always kept in regular telephone contact with mum but chose as soon as I could to live at a distance. Mum lived an isolated but independent life, and after my father left, I supported mum into hospital when she needed it. She never went voluntarily, and I remember coming up to visit the first time I had been involved in mum’s sectioning, and seeing her boarded up door from when the police had broken in so that she could be sectioned. It made me think about how strongly she believed her narratives and how stressful it must have been for her to have that happen. That door, significantly different from the neat row of stained-glass windows in her row of flats, was a reminder of mum’s resistance to hospital long after she stopped being sectioned. I always visited her when a sectioning was to take place after that incident. The build-up to these admissions involved numerous phone calls a day with me, often when I was at work or with friends. No matter how much I asked her if I could phone her later, once mum got on a monologue (she rarely listened to me) it was hard to end the call or reason with mum that she might need to reassess the situation. I rarely did the latter as it ended up with one of us putting the phone down. Mum was admitted to hospital again in 2013 which was the last time she was sectioned. I don’t remember exactly when I realised that mum had dementia but I started to spot that she could not place words and saw her frustration with being unable to form sentences. At her admission to hospital in 2013, I brought it up with the community mental health nurse and mum was seen by a psychologist. She confirmed that mum was finding it hard to place and recall words, and asked if mum would like to be part of a research study but she declined due to her mistrust of health professionals. I was very concerned for mum and had no idea what to expect or what the timeframes were. I was given a booklet on dementia that I remember finding useful, but it still did not address all my concerns. My mother’s medical team spoke to me often of schizophrenia, but conversations about dementia were limited. The booklet certainly did not allow for the personal connection with mum that I was to experience. Mum’s annual reviews from her psychiatrist began to include the diagnosis of mixed dementia alongside complex paranoid schizophrenia but not much changed. I kept in more regular contact – every day, instead of a couple of times a week. I began to notice her cognitive decline.
In 2018, just after I had started a new MSc course, mum had a fall and was admitted to hospital. I rushed up to see her and she was allowed home after a couple of days. She had had several Transient Ischemic Attacks (TIAs, ministrokes). I thought she was going to die, but was reassured when we saw the doctor. However, the TIAs were confirmed as being one of the presentations in the progress of mum’s dementia. It began to feel real and tangible, and I was not sure how I was going to cope with work, a new course, my own health issues, and new responsibilities within the family. Mum had managed independently so far – my brother still went to visit, had his meals cooked, and brought his washing with him. I knew that mum’s condition was worsening when she and my brother phoned to tell me that the washing machine had caught fire, which ended up being a slight exaggeration. I had to phone the fire brigade while they stood and panicked. It was likely to be the graduates – throughout the time that mum had lived in her flat, she was convinced that the graduates were contaminating her food and water, and stealing items. The neighbours were complicit in helping the graduates to do it. In some ways this was a much more simplified narrative from the one from earlier in her life that involved my father, a local clergyman, a solicitor and their related friends and colleagues who in turn informed the whole town what was going on. At the height of her episodes, The Home Office, Radio 3 and a well-known BBC radio newsreader were involved.
Mum began hoarding food, keeping her valuables under her pillow, and rarely leaving the house. I started to have food delivered to her including microwave meals, and my visits to her increased while my brother’s visits began to decrease. Where did the dementia start and the schizophrenia stop, and were the two interacting?
Part 2 and Part 3 of this blog series are now available:
Part 2– Living independently at home as dementia progressed
Part 3 - Living in a care home

Helen Sloan is Public Contributor in National Institute for Health and Care Research for Clinical Research Network Wessex, Clinical Research Network Coordinating Centre, Applied Research Collaboration Wessex Mental Health Hub, and Be Part of Research Advisory Group. She is also part of Wessex Public Involvement Network and a member of the Clinical Trials Group at University of Southampton. She worked as a curator of art, science and technology collaborations for twenty five years before gaining an MSc in Psychology and training to be a Mental Health, Mental Capacity and Care Act Advocate.
All comments and opinions are her own and do not represent any other organisation or individual.
Helen.sloan@nihr.ac.uk
Relevant research and information
Patients with lack of insight into paranoid schizophrenia and admission to hospital
Lehrer, D.S. and Lorenz, J. (2014) ‘Anosognosia in Schizophrenia: Hidden in Plain Sight’, Innovations in Clinical Neuroscience 11(5/6): 10 - 17
Narratives in paranoid schizophrenia
Conneely, M., McNamee, P., Gupta, V., Richardson, J., Priebe, S., Jones, J.M. and Giacco, D. (2020) ‘Understanding Identity Changes in Psychosis: A Systematic Review and Narrative Synthesis.’ The Schizophrenia Bulletin 47(2): 309 – 322
Cowan, H.R., Mittal, V.A. and McAdams, D.P. (2021) ‘Narrative Identity in the Psychosis Spectrum: A Systematic Review and Developmental Model.’ Clinical Psychology Review 88(8) Article 102067
History of medication for schizophrenia and the side effects
Carpenter, W. and Koenig, J.I. (2008) ‘The Evolution of Drug Developments in Schizophrenia Past Issues and Future Opportunities.’ Neuropsychopharmacology 33: 2061 – 2079
National Institute for Health and Care Excellence (NICE) (2014) Psychosis and Schizophrenia in Adults: Treatment and Management [Online] [Accessed 21/09/2023] https://www.nice.org.uk/guidance/cg178/evidence/full-guideline-490503565
Taylor, D.M., Barnes, T.R.E., and Young, A.H. (2021) The Maudsley Prescribing Guidelines in Psychiatry 14th Edition, Chichester: Wiley Blackwell
Impact of upbringing by schizophrenic mother on siblings and children
Fekadu, W., Mihiretu, A., Craig, T.K.J. and Fekadu, A. (2019) ‘Multidimensional impact of severe mental illness on family members: A systematic review.’ British Medical Journal Open [Online] [Accessed 21/09/2023] https://bmjopen.bmj.com/content/bmjopen/9/12/e032391.full.pdf (.PDF)
Duncan, G. and Browning, J. (2009) ‘Adult Attachment in Children Raised by Parents with Schizophrenia.’ Journal of Adult Development 16: 76 – 86
Singhai, K., Jayarajan, D. and Thirthalli, J. (2022) ‘Unmet needs of Children of Parents with Schizophrenia: Need for Global Perspective.’ Journal of Psychosocial Rehabilitation and Mental Health 9: 3 – 6
Early Signs of Dementia and Diagnosis
Alzheimer’s Association (2023) ‘Vascular Dementia.’ [Online] [Accessed 21/09/2023] https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/vascular-dementia
Gamble, L.D., Matthews, F.D., Jones, I.R., Hillman, A.E., Woods, B., Macleod, C.A., Martyr, A., Collins, R., Pentecost, C., Rusted, J.M. and Clare, L. (2022) ‘Characteristics of people living with undiagnosed dementia: findings from the CFAS Wales study.’ BioMed Central Geriatrics 22: 409
Porsteinsson, A.P., Isaacson, R.S., Knox, S. Sabbagle, M.N. and Rubino, I. (2021) ‘Diagnosis of Early Alzheimer’s Disease: Clinical Practice in 2021.’ Journal of Prevention of Alzheimer’s Disease 3(8): 371 - 386
Social Care Institute of Excellence (2020) ‘Early Signs of Dementia.’ [Online] [Accessed 21/09/2023] https://www.scie.org.uk/dementia/
Family reaction to dementia diagnosis and its progress
Chen, M-C. and Lin, H-R. (2022) ‘The experiences of family caregivers in response to a dementia diagnosis disclosure.’ BioMed Centra Psychiatry [Online] [Accessed 21/09/2023]22:409 https://doi.org/10.1186/s12888-022-04126-4
Clemennsen, T.H., Busted, L.M., Seborg, J. and Broun, P. (2019) ‘The family’s experience of phases and roles in the progression of dementia: An explorative interview-based study.’ Dementia 18(2): 490 – 513
Healthtalk.org (2019) ‘Caring for someone with dementia – the experience of carers catalyst film.’ [Online] [Accessed 21/09/2023] https://healthtalk.org/Caring-for-someone-with-dementia---the-experience-of-carers-catalyst-film
Anti-psychotic medications and connection with dementia
Jonas, K., Abi-Dargham, A. and Kotov, R. (2021) ‘Two Hypotheses on the High Incidence of Dementia in Psychotic Disorders.’ Journal of Amencan Medical Association 78(12): 1305 - 1306
TIAs and dementia
Tariq, S., d’Esterre, C.D., Sajobi, T.T., Smith, E.E., Longman, R.S., Frayne, R., Coutts, S.B., Forkert, N.D. and Barber, P.A (2018) ‘A longitudinal magnetic resonance imaging study of neurodegenerative and small vessel disease, and clinical cognitive trajectories in non demented patients with transient ischemic attack: the PREVENT study.’ BioMed Central Geriatrics 28:163
Wardlaw, J.M., Doubal F.., Brown, R., Backhouse, E., Woodhouse L., Bath P., Quinn T.J., Robinson, T., Markus, H.S. , McManus,R., O’Brien, J.T., Werring, D.J., Sprigg, N., Parry-Jones A., Touyz, R.M., Williams,S., Mah, Y-H., Emsley,H. and the R4VaD Investigators (2021) ‘Rates, risks and routes to reduce vascular dementia (R4Vad), a UK wide multicentre prospective observational cohort study of cognition after stroke: Protocol’ European Stroke Journal 6(1): 89 – 1010
Dementia and schizophrenia dual diagnosis
Note, I can find very little on how the two present together. If anyone has any papers to send please let me know. Or perhaps there is a gap in the research here? I will keep looking and post more if I find it in the next blogs.
Cai, L. and Huang, J. (2018) ‘Schizophrenia and risk of dementia: a meta-analysis study.’ Neuropsychiatric Disease and Treatment 14: 2047 - 2055
Hoarding and dementia
Avers, C.R., Najmi, S., Mayes, T.L. and Dozier, M.E. (2015) ‘Hoarding in Older Adulthood.’ The American Journal of Geriatric Psychiatry 23(4): 416 – 422
Trust and dementia
Wong, S., Irish, M., O’Callaghan, C., Kumfor, F., Savage, G., Hodges, J.R., Piguet, O. and Hornberger, M. (2017) ‘Should I trust you? Learning and memory of social interactions in dementia.’ Neuropsychologia 104: 157 - 167


